The following is a conversation with Dr. Henry about working in the mental health field and tips on improving mental health every day.

Dr. Doug Henry Q&A
Vice President and Medical Director, Enterprise Behavioral Health, Highmark Health
Doug Henry, Ph.D., is a licensed clinical psychologist in Pennsylvania and California with a career dedicated to transforming mental health care. Drawn to the integrated payer-provider model and its focus on patient-centered care, Dr. Henry joined the Allegheny Health Network (AHN) Psychiatry and Behavioral Health Institute in 2017 as Vice President. He now serves as Vice President and Medical Director for the Enterprise Behavioral Health at Highmark Health, where he leads efforts to expand access to high-quality behavioral health services across the region.
Before joining AHN, Dr. Henry served as Clinical Administrator at the Western Psychiatric Institute and Clinic of UPMC from 2006 to 2017. His work has consistently focused on improving care for individuals and families navigating mental illness and developmental challenges.
Dr. Henry’s leadership aligns closely with the mission of the “Mental Health: Mind Matters” exhibit at Carnegie Science Center—an interactive experience designed to demystify mental health, reduce stigma, and empower individuals with knowledge and empathy. His commitment to education, access, and advocacy makes him a vital voice in the conversation around mental wellness.
Conversation edited for clarity and brevity.
Q: What inspired you to pursue a career in psychiatry and behavioral health?
A: I still have a paper from first grade that responds to the question, “What do you want to be when you grow up?” with the response, “I want to be a Sikolagist.” My aunt, whom I loved and admired, was a psychologist and I wanted to be like her.
Q: You’ve had many professional experiences over the past few decades – what has been the most rewarding part of your work?
A: This is a difficult question because I’ve had so many rewarding opportunities, experiences, and positions. My current role allows me to design and oversee a system that delivers Behavioral Health support for more than 7 million people. When we get our Behavioral Health/Mental Health provider performance data each month, I take great satisfaction – even joy and happiness – when I can see faster recovery and greater health for the individuals and families to whom we provide care.
Q: The “Mental Health: Mind Matters” exhibition at Carnegie Science Center encourages visitors to explore how mental illness affects thoughts, feelings, and behaviors. What common themes have you observed in your clinical work that align with the messages inside the exhibit?
A: The mind-body connection. This exhibit helps young people to overcome the mistaken idea that mental health is somehow different from physical health. We have a unitary experience in life, as opposed to separate physical and mental experiences. It is always both, and they are inseparable. The exhibit does well to show what is happening in the brain and the body when a person has a mental illness and connects that to things that we can do to get well again. When you recognize that mind and body aren’t really separate, it decreases stigma and opens pathways to greater self-control.
Q: One of the goals of “Mental Health: Mind Matters” is to reduce stigma. In your experience, what are the most effective ways to shift public perception and encourage open conversations about mental health?
A: The best stigma reducer is to normalize receiving mental health care or support as an aspect of health hygiene. This often has to do with integrating opportunities to receive mental health treatment alongside other health services like primary care or pediatrics. It also can mean placing these service opportunities where people are accustomed to going, such as school or at work.
Making mental health treatment spaces appealing is another important way that we can reduce stigma. At more than 50 local schools served by Allegheny Health Network’s (AHN) Chill Project, there are behavioral health offices used for individual and family work, but there are also what we call “Chill Rooms.” These are usually classrooms that have been carefully redecorated to create a warm, welcoming, comfortable environment resembling a well-furnished living room. Upon opening our first Chill Room in a large public high school in 2019, we had more than 10,000 self-directed (voluntary) visits within the first six months of operation.
Q: How has the COVID-19 pandemic changed the way we think about and access mental health services?
A: In at least three big ways. First, mental health became a priority on the national landscape in a way that had not before in the United States.
Second, so many of us were impacted by the stress of the pandemic – a normal response to the situation – that many people came to find that mental health stigma is shaped by lack of understanding and knowledge. Things began to change even before the pandemic, as superstar athletes openly discussed psychological struggles, including Michael Phelps, Naomi Osaka, Simone Biles, Chloe Kim, Dak Prescott, and Aaron Rodgers.
Third, the tele-psychiatry and tele-therapy revolution came about out of necessity. Mental health professionals were able to confirm that, in most circumstances, remote treatment was both safe and effective. This continues to enable millions of people to receive care who were previously unable due to transportation difficulties and work requirements.
Q: Mental health professionals often face high levels of stress. What strategies do you personally use to maintain your own mental wellness?
A: This is something that every mental health clinician must discover early in their career to avoid burning out. It’s a difficult thing and each professional must find the unique methods that work best for them.
For me, separating work in concrete ways from other dimensions of life has been essential. For this reason, I always come into the office in the morning five or six days a week, although I have the option of work-from-home days. When I was a young psychologist, the drive home from the hospital or clinic, was an important marker and adjustment period for me to switch gears and become fully present in my personal relationships.
Relationships are the most effective way to convert a lot of dark material (stuff that is happening with and to your patients), into something bearable. Early on, I shared some of the types of challenges I encountered at work with my psychologist partner (protecting patient identity and privacy always). But after beginning a fellowship in a Southern California Medicaid clinic, having the privilege and challenge of seeing 10 patients per day who were often facing the most serious kinds of existential challenges, I realized that I needed to leave work at work. Now, I have found that I can consult with other professionals when I am uneasy about a patient, so that I am not alone with my concerns and so that I have more confidence.
Q: Any other thoughts you’d like to share with the public about the topics presented in the exhibit?
A: I’m so proud of Pittsburgh and pleased that Carnegie Science Center is featuring the “Mental Health: Mind Matters” exhibit. Much of what constitutes mental health is rather difficult to visually depict. The curiosity-provoking and physically engaging nature of the exhibit is unmistakably communicative, reflecting the joint involvement of mind and body throughout all mental health topics.
The exhibit elevates concerns around mental health, includes lessons to reduce stigma, and gives voice to the silent suffering of many. The content is appropriate and accessible to the full range of pre-teens and teenagers while remaining accurate to understandings about mental health which are sometimes complex.

Dr. Doug Henry Q&A
Vice President and Medical Director, Enterprise Behavioral Health, Highmark Health
Doug Henry, Ph.D., is a licensed clinical psychologist in Pennsylvania and California with a career dedicated to transforming mental health care. Drawn to the integrated payer-provider model and its focus on patient-centered care, Dr. Henry joined the Allegheny Health Network (AHN) Psychiatry and Behavioral Health Institute in 2017 as Vice President. He now serves as Vice President and Medical Director for the Enterprise Behavioral Health at Highmark Health, where he leads efforts to expand access to high-quality behavioral health services across the region.
Before joining AHN, Dr. Henry served as Clinical Administrator at the Western Psychiatric Institute and Clinic of UPMC from 2006 to 2017. His work has consistently focused on improving care for individuals and families navigating mental illness and developmental challenges.
Dr. Henry’s leadership aligns closely with the mission of the “Mental Health: Mind Matters” exhibit at Carnegie Science Center—an interactive experience designed to demystify mental health, reduce stigma, and empower individuals with knowledge and empathy. His commitment to education, access, and advocacy makes him a vital voice in the conversation around mental wellness.
Conversation edited for clarity and brevity.
Q: What inspired you to pursue a career in psychiatry and behavioral health?
A: I still have a paper from first grade that responds to the question, “What do you want to be when you grow up?” with the response, “I want to be a Sikolagist.” My aunt, whom I loved and admired, was a psychologist and I wanted to be like her.
Q: You’ve had many professional experiences over the past few decades – what has been the most rewarding part of your work?
A: This is a difficult question because I’ve had so many rewarding opportunities, experiences, and positions. My current role allows me to design and oversee a system that delivers Behavioral Health support for more than 7 million people. When we get our Behavioral Health/Mental Health provider performance data each month, I take great satisfaction – even joy and happiness – when I can see faster recovery and greater health for the individuals and families to whom we provide care.
Q: The “Mental Health: Mind Matters” exhibition at Carnegie Science Center encourages visitors to explore how mental illness affects thoughts, feelings, and behaviors. What common themes have you observed in your clinical work that align with the messages inside the exhibit?
A: The mind-body connection. This exhibit helps young people to overcome the mistaken idea that mental health is somehow different from physical health. We have a unitary experience in life, as opposed to separate physical and mental experiences. It is always both, and they are inseparable. The exhibit does well to show what is happening in the brain and the body when a person has a mental illness and connects that to things that we can do to get well again. When you recognize that mind and body aren’t really separate, it decreases stigma and opens pathways to greater self-control.
Q: One of the goals of “Mental Health: Mind Matters” is to reduce stigma. In your experience, what are the most effective ways to shift public perception and encourage open conversations about mental health?
A: The best stigma reducer is to normalize receiving mental health care or support as an aspect of health hygiene. This often has to do with integrating opportunities to receive mental health treatment alongside other health services like primary care or pediatrics. It also can mean placing these service opportunities where people are accustomed to going, such as school or at work.
Making mental health treatment spaces appealing is another important way that we can reduce stigma. At more than 50 local schools served by Allegheny Health Network’s (AHN) Chill Project, there are behavioral health offices used for individual and family work, but there are also what we call “Chill Rooms.” These are usually classrooms that have been carefully redecorated to create a warm, welcoming, comfortable environment resembling a well-furnished living room. Upon opening our first Chill Room in a large public high school in 2019, we had more than 10,000 self-directed (voluntary) visits within the first six months of operation.
Q: How has the COVID-19 pandemic changed the way we think about and access mental health services?
A: In at least three big ways. First, mental health became a priority on the national landscape in a way that had not before in the United States.
Second, so many of us were impacted by the stress of the pandemic – a normal response to the situation – that many people came to find that mental health stigma is shaped by lack of understanding and knowledge. Things began to change even before the pandemic, as superstar athletes openly discussed psychological struggles, including Michael Phelps, Naomi Osaka, Simone Biles, Chloe Kim, Dak Prescott, and Aaron Rodgers.
Third, the tele-psychiatry and tele-therapy revolution came about out of necessity. Mental health professionals were able to confirm that, in most circumstances, remote treatment was both safe and effective. This continues to enable millions of people to receive care who were previously unable due to transportation difficulties and work requirements.
Q: Mental health professionals often face high levels of stress. What strategies do you personally use to maintain your own mental wellness?
A: This is something that every mental health clinician must discover early in their career to avoid burning out. It’s a difficult thing and each professional must find the unique methods that work best for them.
For me, separating work in concrete ways from other dimensions of life has been essential. For this reason, I always come into the office in the morning five or six days a week, although I have the option of work-from-home days. When I was a young psychologist, the drive home from the hospital or clinic, was an important marker and adjustment period for me to switch gears and become fully present in my personal relationships.
Relationships are the most effective way to convert a lot of dark material (stuff that is happening with and to your patients), into something bearable. Early on, I shared some of the types of challenges I encountered at work with my psychologist partner (protecting patient identity and privacy always). But after beginning a fellowship in a Southern California Medicaid clinic, having the privilege and challenge of seeing 10 patients per day who were often facing the most serious kinds of existential challenges, I realized that I needed to leave work at work. Now, I have found that I can consult with other professionals when I am uneasy about a patient, so that I am not alone with my concerns and so that I have more confidence.
Q: Any other thoughts you’d like to share with the public about the topics presented in the exhibit?
A: I’m so proud of Pittsburgh and pleased that Carnegie Science Center is featuring the “Mental Health: Mind Matters” exhibit. Much of what constitutes mental health is rather difficult to visually depict. The curiosity-provoking and physically engaging nature of the exhibit is unmistakably communicative, reflecting the joint involvement of mind and body throughout all mental health topics.
The exhibit elevates concerns around mental health, includes lessons to reduce stigma, and gives voice to the silent suffering of many. The content is appropriate and accessible to the full range of pre-teens and teenagers while remaining accurate to understandings about mental health which are sometimes complex.
To stay updated on the latest science news from Carnegie Science Center, make sure to sign up ![]() to receive updates and never miss science news.
to receive updates and never miss science news.
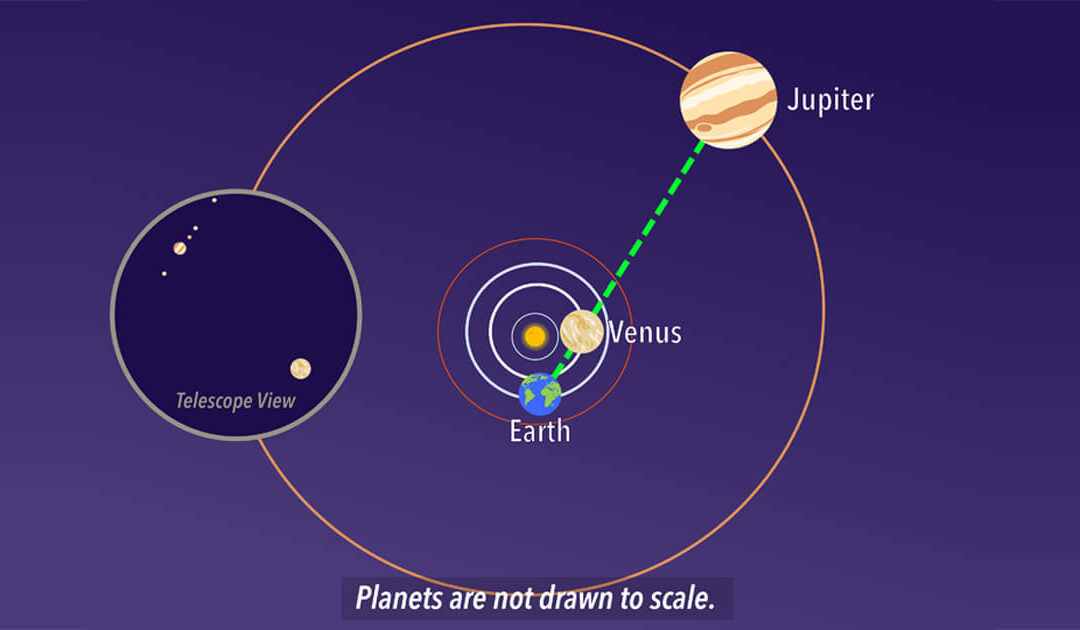
Stargazing: Perseids and Venus-Jupiter Conjunction
This time of year is usually the moment to break out the lawn chairs for the annual spectacle of the Perseid meteor shower. Home > Blog ...
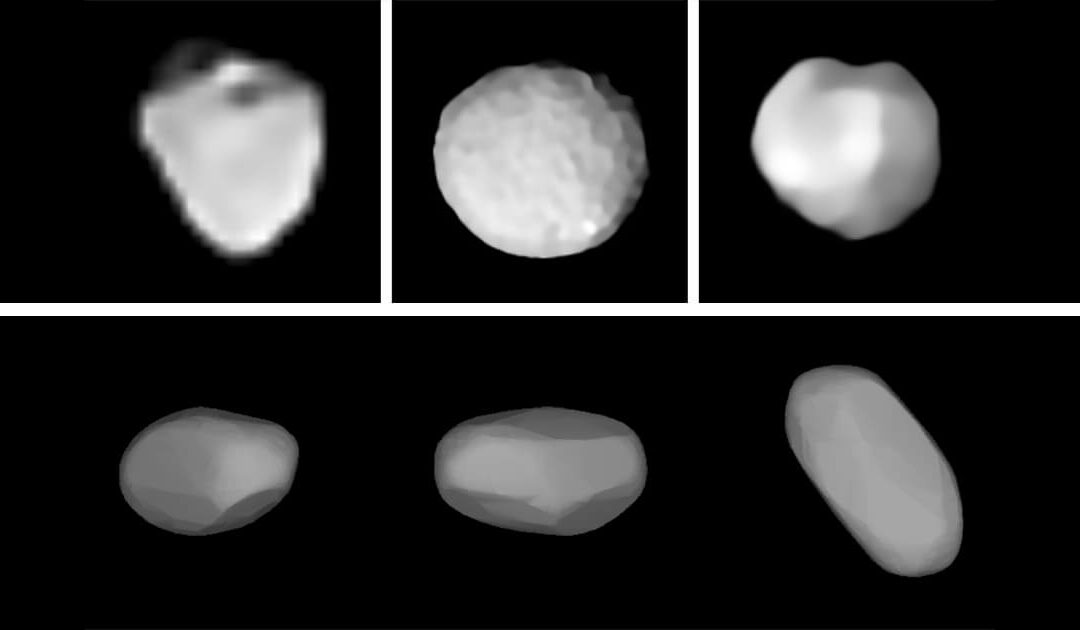
Stargazing: August Asteroids
Several large asteroids will have their brightest showings of the year through August. Home > Blog Between the planetary orbits...

Stargazing: Crescent Moon by Spica
On the evening of July 30, one of the bluest stars in the sky will gleam just above the waxing crescent moon. Spica is a blue giant star and the brightest in the constellation Virgo. Home > Blog [acf...

Stargazing: Scorpius
Soaring through July skies is an ancient arachnid known for its sting. Scorpius the Scorpion, with its distinctive curved spine and stinger poised to strike, holds a large profile low to the southern horizon. Its Latin name translates to the “creature with the...

Stargazing: Vega – Anniversary of First Photo of Star Taken
On July 17th, 1850, the first photograph of a star other than our Sun was taken. Home > Blog Brilliant Vega is the brightest...

Stargazing: Pittsburgh Goes to the Moon
This year celebrates the 56th anniversary of the first moon landing. On July 20, the world watched as Neil Armstrong and Buzz Aldrin stepped onto the surface of the moon. Home > Blog [sv...

Dr. Amy Welsh Q&A
The following is a conversation with Dr. Amy Welsh about her background and her perspective on the sensational dire wolf story. Home > Blog Dr. Amy Welsh Q&A West Virginia University School of Natural...
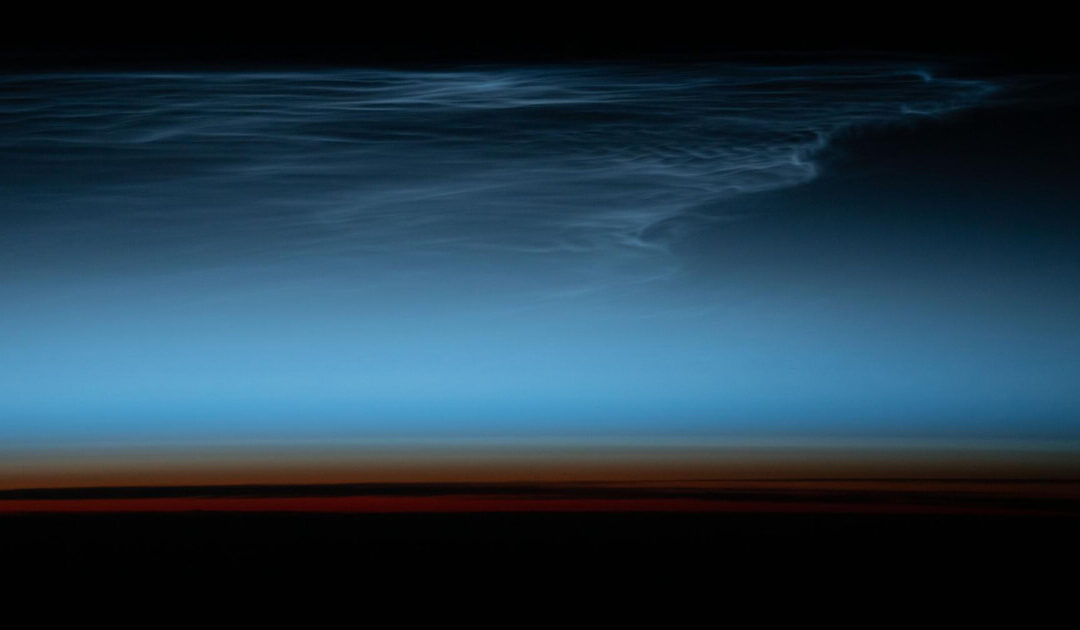
Stargazing: Noctilucent Clouds
Summer is the season to spot rare and luminescent Noctilucent Clouds. From May to early August, these ethereal clouds show their best displays thirty minutes after sunset or before sunrise. Home > Blog [acf...
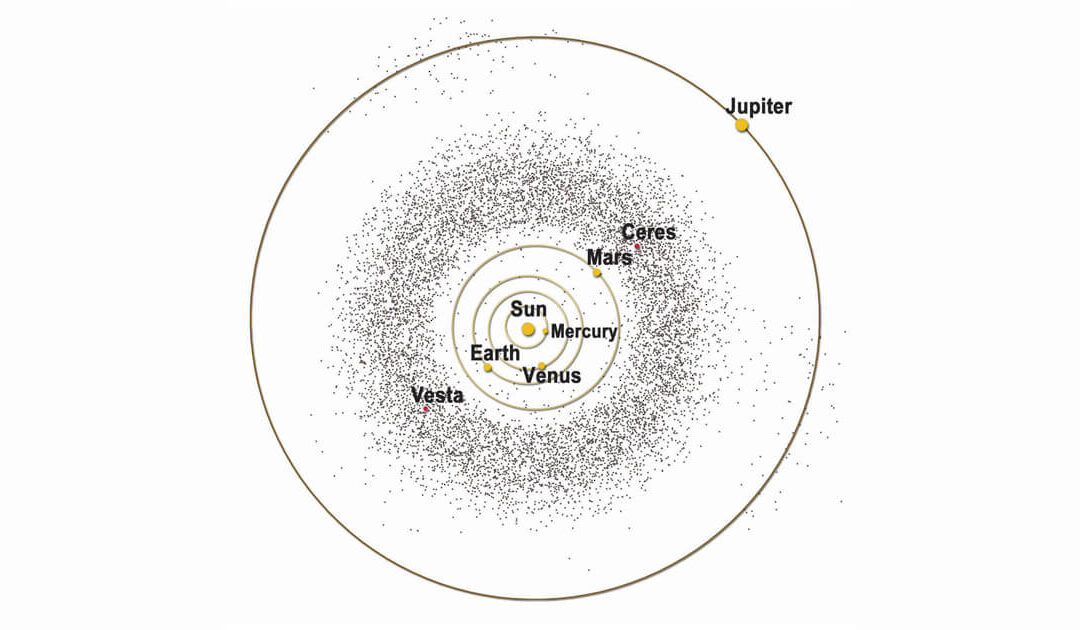
Stargazing: June 30 Asteroid Day – date of Siberian Tunguska Event
Pre-dawn hours of June 27 will bring peak opportunities to view June’s Bootid meteor shower. A thin crescent moon will enhance the chances of seeing meteors flash across the sky. Home > Blog ...

Stargazing: Solstice June 20– also, Moon-Saturn-Neptune close approach 5:45 a.m. June 18
Welcome summer! On Friday June 20 at 10:42 p.m. EDT, the sun will reach its northern-most point in the sky. Home > Blog Welcome...


